
How Do I Know If I Have a Cavity — and What Can I Do About It?
Key Takeaways
- A dental cavity is a permanently damaged area in the enamel that develops into tiny holes due to bacteria, acid, and poor oral hygiene.
- Cavities begin silently and may not show obvious symptoms in early stages.
- Early warning signs include mild sensitivity and small discoloured spots; advanced cavities can cause intense pain and even infection.
- Self-checks can help identify potential cavities, but professional dental exams remain crucial.
What exactly is a dental cavity, and how does it form?
Imagine biting into a cold treat and feeling a tiny zap in your tooth. That could be a warning sign of a cavity — technically known as dental caries. But what exactly is a cavity, and why does it happen?
A cavity is a small hole or opening in the surface of a tooth caused by tooth decay, a process initiated by bacterial activity in the mouth. The enamel — the tooth’s outermost protective layer — is gradually broken down by acids produced by bacteria feeding on sugars.
How it starts: Plaque, bacteria, and acid
It all begins with dental plaque, a sticky biofilm that forms when bacteria in the mouth mix with food particles and saliva. When you consume carbohydrates — especially sugars — the bacteria in plaque convert these into acid. Over time, the repeated acid attacks erode the enamel, leading to demineralization and, eventually, the formation of a cavity.
The Canadian Dental Association (CDA) explains that without proper oral hygiene, plaque can harden into tartar, further complicating the decay process. According to research from the National Institutes of Health (NIH), tooth decay is one of the most prevalent chronic diseases globally, especially in children and adolescents.
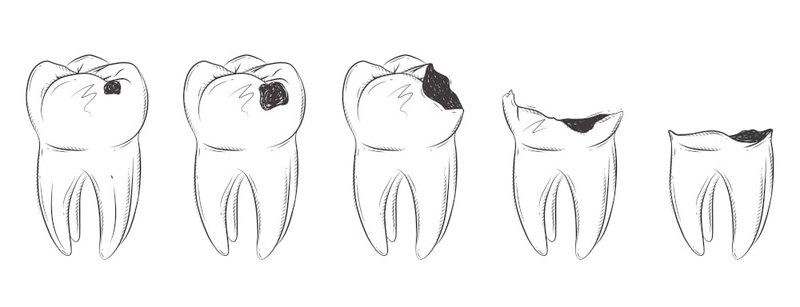
Stages of cavity formation
- Initial demineralization: Acid begins to leach minerals from the enamel.
- Enamel decay: The surface of the enamel breaks down.
- Dentin exposure: Bacteria reach the softer dentin layer beneath the enamel.
- Pulp involvement: Infection reaches the tooth pulp, causing pain and potentially leading to an abscess..
"Dental caries are entirely preventable with routine brushing, proper diet, and regular dental visits." — Dr. James C.H. Ko, DDS
How can you tell if you have a cavity at home?
Cavities don’t always announce themselves with pain — especially not in their early stages. But there are several subtle clues your teeth may be giving you.
Early signs to watch for
- Tooth sensitivity when consuming hot, cold, or sweet items
- Visible spots on teeth — white, brown, or black
- Bad breath or a persistent, unpleasant taste in the mouth
- Rough or jagged edges felt with the tongue.
- Mild discomfort while chewing or brushing a specific area
These signs can indicate the start of enamel erosion, which may evolve into a cavity if left untreated.
Self-check tips
While a dental exam is the only way to confirm a cavity, some at-home techniques can raise red flags:
- Use a mirror and flashlight to inspect the chewing surfaces of molars.
- Look for visible pits or holes in the enamel.
- Check for dark spots that don’t brush off easily.
- Gently press your fingernail on suspect areas to detect softness or tenderness.
What does a cavity feel like in its early stages vs later stages?
One of the trickiest aspects of cavities is that they may start without any pain at all. That’s why it’s essential to understand the different sensations associated with early vs advanced cavities.
Early-stage cavity symptoms
- Mild sensitivity to temperature changes
- No visible holes, only faint white or brown patches
- Dull discomfort, usually intermittent
- No swelling or visible inflammation
At this stage, decay is limited to the enamel and can often be reversed or treated with non-invasive methods, such as fluoride varnish.
Advanced-stage cavity symptoms
- Sharp, persistent pain — especially when chewing or exposed to temperature extremes
- Visible holes or pits in the tooth
- Swelling around the affected tooth
- Dark discolouration spreading across the enamel.
- Bad breath or metallic taste
These symptoms occur when the decay reaches the dentin or pulp, where nerve endings reside. At this point, more invasive treatments, such as fillings, root canals, or even extractions, may be necessary.
Symptom comparison table
| Symptom | Early Stage | Advanced Stage |
|---|---|---|
| Tooth Sensitivity | Mild, intermittent | Sharp, lingering |
| Visible Tooth Changes | White or faint brown spots | Dark brown/black pits or holes |
| Pain Level | Low discomfort | Severe pain during chewing |
| Gum/Soft Tissue Involvement | None | Possible swelling or tenderness |
| Treatment Required | Remineralization, fluoride | Fillings, root canal, extraction |
What dentists advise not to ignore
Dentists emphasize the importance of not waiting until pain occurs. Regular dental checkups and cleanings help detect cavities in their earliest stages.
How do dentists diagnose cavities during a check-up?
While self-checks are helpful, professional dental assessments provide a much more precise and accurate picture. Dentists use a combination of tools and techniques to detect cavities at various stages of development.
Key diagnostic tools
- Visual examination: Dentists start by inspecting teeth under bright lights, looking for discoloration, surface roughness, or obvious holes.
- Dental explorer/probe: A pointed instrument helps test the tooth’s surface for soft or sticky areas, which may indicate decay.
- X-rays (radiographs): Bitewing X-rays reveal cavities between teeth or beneath the surface, where visual checks fall short.
- Laser fluorescence devices: Some clinics use tools like DIAGNOdent, which can detect hidden caries via light reflection.
The Canadian Dental Association recommends routine X-rays based on age and cavity risk level. These images are crucial in identifying decay in its earliest, most treatable stages.
"X-rays help us see what the eye can’t. Even a tooth that looks perfect on the outside might be hiding deep decay." — Dr. Jerry Jesin, DDS
Frequency of check-ups
Most dentists recommend a check-up every six months, but patients with higher risk may need more frequent visits. Children, those with a history of decay, and individuals with orthodontic appliances are particularly advised to stick to regular exams.
What causes dental decay, and how can you prevent it?
Dental decay doesn’t happen overnight. It’s the result of a continuous battle between acid attacks and your body’s ability to repair enamel. Understanding both the causes and the prevention methods helps reduce risk.
Significant causes of dental decay
- High sugar consumption: Sugary foods feed acid-producing bacteria.
- Poor oral hygiene: Infrequent brushing or flossing allows plaque to build up.
- Low saliva production: Saliva neutralizes acids; dry mouth increases the risk of cavities.
- Acidic pH levels: Foods and drinks that lower pH can erode enamel over time.
- Deep tooth grooves: Molars with deep fissures are more prone to trapping food and bacteria.
How to prevent tooth decay
- Brush twice daily with fluoride toothpaste.
- Floss daily to remove plaque from between teeth
- Use mouthwash with antibacterial properties.
- Limit sugary snacks and drinks, especially between meals.
- Stay hydrated to support saliva production.
- Visit the dentist regularly for cleanings and exams.
Causes vs Prevention: A comparison table
| Causes of Decay | Prevention Strategies |
|---|---|
| High sugar intake | Limit sugars; rinse mouth after eating |
| Poor oral hygiene | Brush/floss twice daily |
| Acidic food and beverages | Use a straw, rinse with water |
| Dry mouth | Stay hydrated, chew sugar-free gum |
| Skipping dental visits | Schedule check-ups every 6 months |

What are the symptoms of tooth decay that most people ignore?
Cavities don’t always scream for attention. In fact, some of the most telling signs are the ones patients often dismiss as minor or unrelated.
Subtle but essential symptoms
- Chronic bad breath (halitosis) despite brushing
- Slight discoloration that gradually darkens
- Mild temperature sensitivity that comes and goes
- Tiny cracks or chips in the enamel
- Unusual taste in the mouth, often metallic or sour
These signs are commonly overlooked or attributed to dietary issues. However, they often reflect early-stage decay that can be easily treated if caught in time.
Clinical warning signs shared by dentists
- Recurring sensitivity in the same spot
- Pain when flossing between specific teeth
- Gums pulling away from the tooth (a potential entry point for decay)
- Discomfort when biting down, even without visible damage
These warning signs are often reported in the early stages of decay, when intervention is most effective. That’s why dentists advocate for not waiting until pain becomes noticeable.
What happens if you don’t treat a cavity?
Skipping dental visits or ignoring that nagging tooth sensitivity can set off a chain reaction. What begins as a microscopic lesion in your enamel can evolve into a serious — and painful — problem. Here's what happens when a cavity is left untreated.
Timeline of untreated decay
- Initial enamel erosion: At this stage, the cavity is still reversible with fluoride treatments.
- Dentin involvement: The decay spreads beneath the enamel, exposing the tooth’s softer inner layer. This stage usually triggers sensitivity and mild pain.
- Pulp infection: Bacteria reach the nerve-rich pulp, leading to inflammation and, in some cases, severe pain.
- Abscess formation: Infection can form a pus-filled pocket at the root of the tooth, often accompanied by swelling and fever.
- Tooth loss and systemic spread: If untreated, the infection may destroy the bone supporting the tooth or even spread to other parts of the body.
Serious health risks from untreated decay
- Tooth fracture or total loss: The tooth structure becomes too weak to support chewing.
- Gum infection (periodontitis): Untreated cavities near the gumline can lead to inflammation and the spread of bacteria.
- Jawbone damage: Chronic infection can cause the surrounding bone to deteriorate.
- Sepsis: In rare cases, dental infections can lead to bloodstream infections that affect vital organs.

What’s the difference between dental decay and tooth caries?
It’s easy to use the terms dental decay and tooth caries interchangeably — and often, people do. However, in clinical dentistry, the distinction can be significant depending on the context.
Terminology comparison used in clinical dentistry
| Term | Definition | Usage Context |
|---|---|---|
| Dental Decay | A general term for the breakdown of tooth structure due to acids from plaque bacteria. | Commonly used in patient education and public health. |
| Tooth Caries | A specific pathological process involving localized demineralization and destruction of enamel/dentin. | Preferred in research, diagnostics, and academic writing. |
How they relate
- Dental decay refers broadly to the disease process that leads to the breakdown of enamel.
- Caries describes the actual lesion or the result of that decay process.
Why the distinction matters
Understanding both terms improves communication between dental professionals and patients. When your dentist says you have “incipient caries,” they’re referring to early-stage decay that may still be reversible. Knowing the vocabulary helps patients better understand their treatment options and the severity of their condition.
How do you protect your enamel from future cavities?
Cavity prevention doesn’t just stop at brushing. Long-term enamel protection is a combination of good habits, a balanced diet, and regular professional care. Here’s how to proactively shield your teeth from future damage.
Best daily practices
- Brush with fluoride toothpaste twice a day — fluoride helps remineralize enamel.
- Floss daily to remove plaque and food between teeth.
- Use an alcohol-free fluoride rinse to add a protective layer against acid.
- Avoid frequent snacking, especially sugary or acidic foods.
- Drink plenty of water, especially fluoridated tap water.
Smart dietary choices
- Limit acidic beverages, such as soda, citrus juices, and wine.
- Eat calcium-rich foods (cheese, yogurt) to strengthen enamel.
- Chew sugar-free gum to stimulate saliva production.
- Avoid sticky candies that cling to molars.
Professional enamel protection
- Dental sealants: Thin coatings applied to molars to prevent food from getting stuck in grooves.
- Fluoride treatments Are Offered during routine cleanings to strengthen enamel.
- Regular check-ups: Dentists can detect early enamel erosion before it develops into a cavity.
Topic-specific table: Protecting enamel effectively
| Enamel Protection Strategy | How It Works | Recommended Frequency |
|---|---|---|
| Brushing with fluoride | Remineralizes enamel and neutralizes acid | 2x daily |
| Flossing | Removes interdental plaque | 1x daily |
| Dental sealants | Shields grooves on molars | Every 5–10 years (as needed) |
| Fluoride varnish/rinse | Provides a protective mineral barrier | Every 3–6 months professionally |
| Avoiding acidic foods/drinks | Reduces erosion and acid exposure | Daily dietary management |
What should you do if you suspect a cavity right now?
If you’ve noticed a spot on your tooth or feel sudden sensitivity when drinking cold water, don’t wait. Cavities can develop quickly, and early treatment is always easier — and less expensive.
Symptoms vs Actions Table
| Symptom Noticed | Recommended Action |
|---|---|
| Mild sensitivity to cold/sweets | Schedule a dental exam |
| Visible white or brown spot | Use fluoride toothpaste, and see your dentist soon |
| Pain while chewing | Call a dentist immediately |
| Bad breath that won’t go away | Consider decay or gum issues — book a check-up |
| Discolouration or pit | Likely decay — prompt professional evaluation |
Treatment options
- Fluoride treatment for early lesions
- Tooth-coloured fillings for small to moderate cavities
- Root canal therapy is necessary if the decay reaches the pulp
- Tooth extraction in severe cases, followed by prosthetic solutions
Expert recommendations
- Don’t delay: Even minor symptoms can signal deeper problems.
- Keep a log of symptoms, including frequency and intensity.
- Don’t self-diagnose: Only a dentist can confirm whether it’s a cavity or something else.
- Commit to prevention: Future cavities can often be avoided with lifestyle changes and professional guidance.
Ultimately, the best course of action is to book a dental appointment as soon as you notice something feels off. Cavities don’t get better on their own — they only get worse.

